Our Division has a long tradition of NIH-sponsored research in ARDS and has played a key role in some of the field’s most important pre-clinical, translational, and clinical studies. We participate in multiple consortiums such as the NHLBI Prevention and Early Treatment of Acute Lung Injury (PETAL), NIAID Strategies and Treatments for Respiratory Infections and Viral Emergencies (STRIVE), the CDC Investigating Respiratory Viruses in the Acute Ill (IVY), and the NIH Strategies to Innovate Emergency Care Clinical Trials Network (SIREN) Network and collaborate extensively with other UW Departments including Surgery, Biomedical Engineering, and Radiology. We conduct research at the Center for Lung Biology on the UW South Lake Union Campus (pre-clinical studies) and translational/clinical studies at Harborview Medical Center in Downtown Seattle, WA.
Our Division has a long tradition of NIH-sponsored research in ARDS and has played a key role in some of the field’s most important pre-clinical, translational, and clinical studies. We participate in multiple consortiums such as the NHLBI Prevention and Early Treatment of Acute Lung Injury (PETAL), NIAID Strategies and Treatments for Respiratory Infections and Viral Emergencies (STRIVE), the CDC Investigating Respiratory Viruses in the Acute Ill (IVY), and the NIH Strategies to Innovate Emergency Care Clinical Trials Network (SIREN) Network and collaborate extensively with other UW Departments including Surgery, Biomedical Engineering, and Radiology. We conduct research at the Center for Lung Biology on the UW South Lake Union Campus (pre-clinical studies) and translational/clinical studies at Harborview Medical Center in Downtown Seattle, WA.
Pre-clinical research
Drs. Anne Manicone, Chi Hung, and Bill Altemeier conduct laboratory-based research using relevant mouse models of acute lung injury with genetic knockouts and state-of-the-art molecular, physiologic, and histologic analyses. Each of these groups have extensive collaborations with translational and clinical researchers.
genomics and bioinformatics
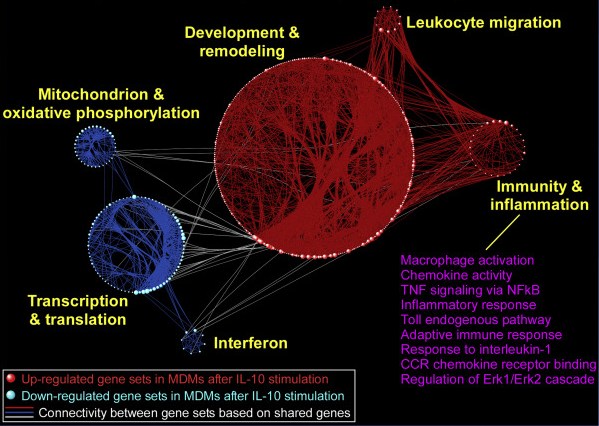
Dr. Sina Gharib is the Director of the Computational Medicine Core at the UW Center for Lung Biology. Dr. Gharib has extensive experience in applying systems biology and state-of-the-art computational methods based on pathway and network analyses of ARDS and critical illness in both animal and human studies. Dr. Mark Wurfel is a genetic epidemiologist with expertise in determining genetic susceptibility to ARDS and other critical illness syndromes.
translational research
Drs. Pavan Bhatraju, Linzee Mabrey, Neha Sathe, Mark Wurfel, and Eric Morrell conduct translational research focused on the molecular epidemiology of ARDS in close collaboration with several other programs including the lab of Carmen Mikacenic at the Benaroya Research Institute (BRI). They enroll patient cohorts from the ICU and utilize biologic data generated from these cohorts to define high-risk groups and treatment-responsive subgroups of ICU syndromes.
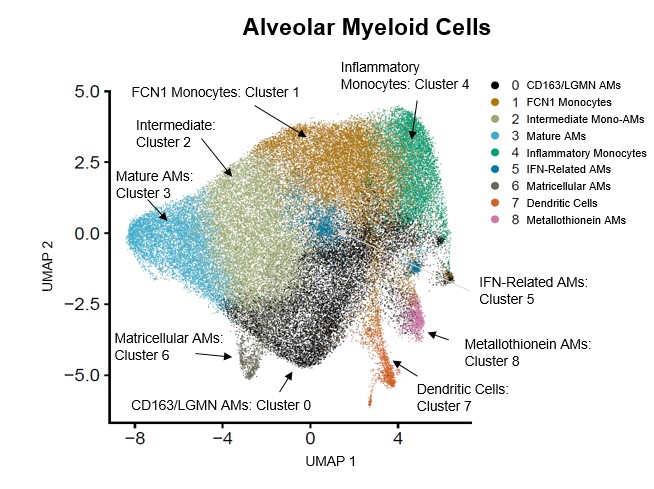
Over the past 25 years, the University of Washington has been a leader in utilizing lower respiratory tract sampling from patients with ARDS to understand the molecular determinants of disease. Current NIH-funded projects include studies on alveolar macrophage subsets and ontogeny in ARDS; role of the CD14-pathway in ARDS; and lung-specific subphenotypes of disease.
clinical/epidemiology research

Our Division was involved in some of the earliest studies describing the epidemiology of ARDS. Dr. Neha Sathe applies biostatistical and machine-learning approaches to electronic health records to risk-stratify patients with ARDS and similar forms of respiratory failure. Dr. Nick Johnson focuses on the epidemiology of ARDS after out-of-hospital cardiac arrest.
interventional trials
The UW Division of Pulmonary, Critical Care Division has been at the forefront of clinical trials for ARDS for more than three decades. The Division has played an integral role in the National Heart, Lung, and Blood Institute (NHLBI) ARDS Network and its successor, the PETAL Network.
Currently, Drs. Nick Johnson and Linzee Mabrey direct the ARDS interventional trials group. Together, they lead an interdisciplinary team that includes key collaborators such as Drs. Eric Morrell and Mark Wurfel, faculty partners from the Departments of Surgery and Emergency Medicine, and a team of research coordinators.
The team's research efforts focus on several cutting-edge areas. One major area of investigation is the identification and implementation of personalized ventilation strategies. Recognizing the heterogeneity of ARDS, the group strives to tailor mechanical ventilation approaches to the individual physiology of each patient, thereby reducing lung injury and improving outcomes. These innovative strategies consider factors such as lung compliance, inflammation, and oxygenation requirements to optimize respiratory support. Another central theme of their research is immune modulation in ARDS. The team's work aims to better understand the immune dysregulation that underpins ARDS and its progression. By targeting specific pathways involved in inflammation and immune response (e.g. CD14-related pathways), we are investigating novel therapeutic interventions that could mitigate lung injury and systemic effects of the disease. Through its involvement in both investigator-initiated and multicenter clinical trials, the Division remains steadfast in its mission to pioneer advancements in the treatment of ARDS.